Breast Screening
Be breast aware
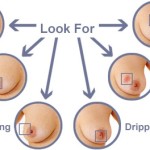
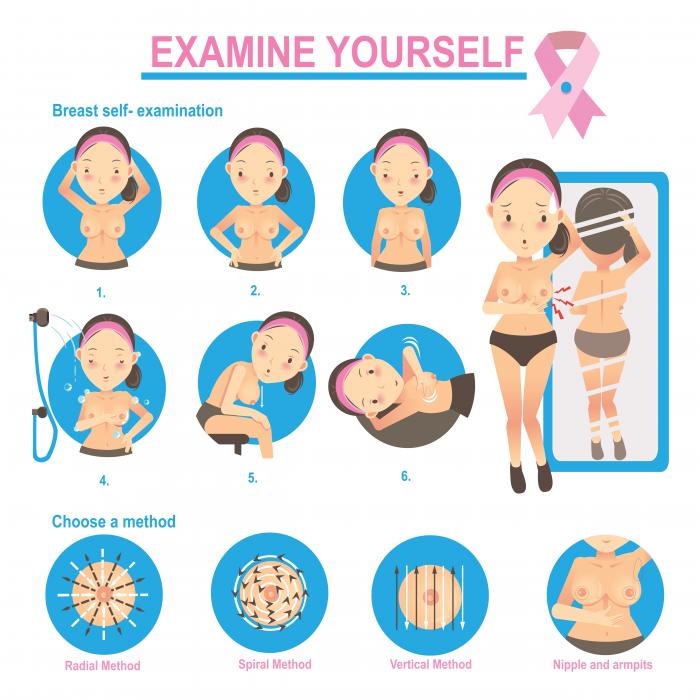
Women should be ‘breast aware’ and check their breasts regularly. Breast awareness means being familiar with your breasts and what is normal for them so you can recognise any changes easily and quickly. If you notice a lump on your breast, or any change in its appearance, feel or shape, you should have it checked by your doctor as soon as possible.
The advice below may help you to become ‘breast aware’:
- You can feel your breasts whilst lying down in bed or in the bath or shower using a soapy hand. Using body lotion can help. It is important to feel the whole breast, including the armpit.
- You can look at your breasts in the mirror. Move your arms above your head, onto your hips or by your sides so you can see your breasts from every angle, including the underside.
- As older women are at greater risk of developing breast cancer, it is very important to be aware of any unusual changes after the menopause (when your periods stop.)
Breasts may change with age and life events, such as pregnancy, breastfeeding, during your periods and after the menopause. This is why it is important to know what is normal for you so you will recognize any changes.
Questionnaire:
Common types of benign breast lumps include:
- should not increase your risk of developing breast cancer in the future
- If a lump is present, when did you first notice the lump?
- Do you have any other symptoms, such as pain or a discharge from your nipple?
- Do your symptoms change with your menstrual cycle?
- Have you have ever injured your breast?
- Do you have any risk factors for breast cancer, such as a close family member who has previously had breast cancer?
- What medications you are currently taking?
- Are you are currently breastfeeding or have you done so in the past?
When to see your doctor:
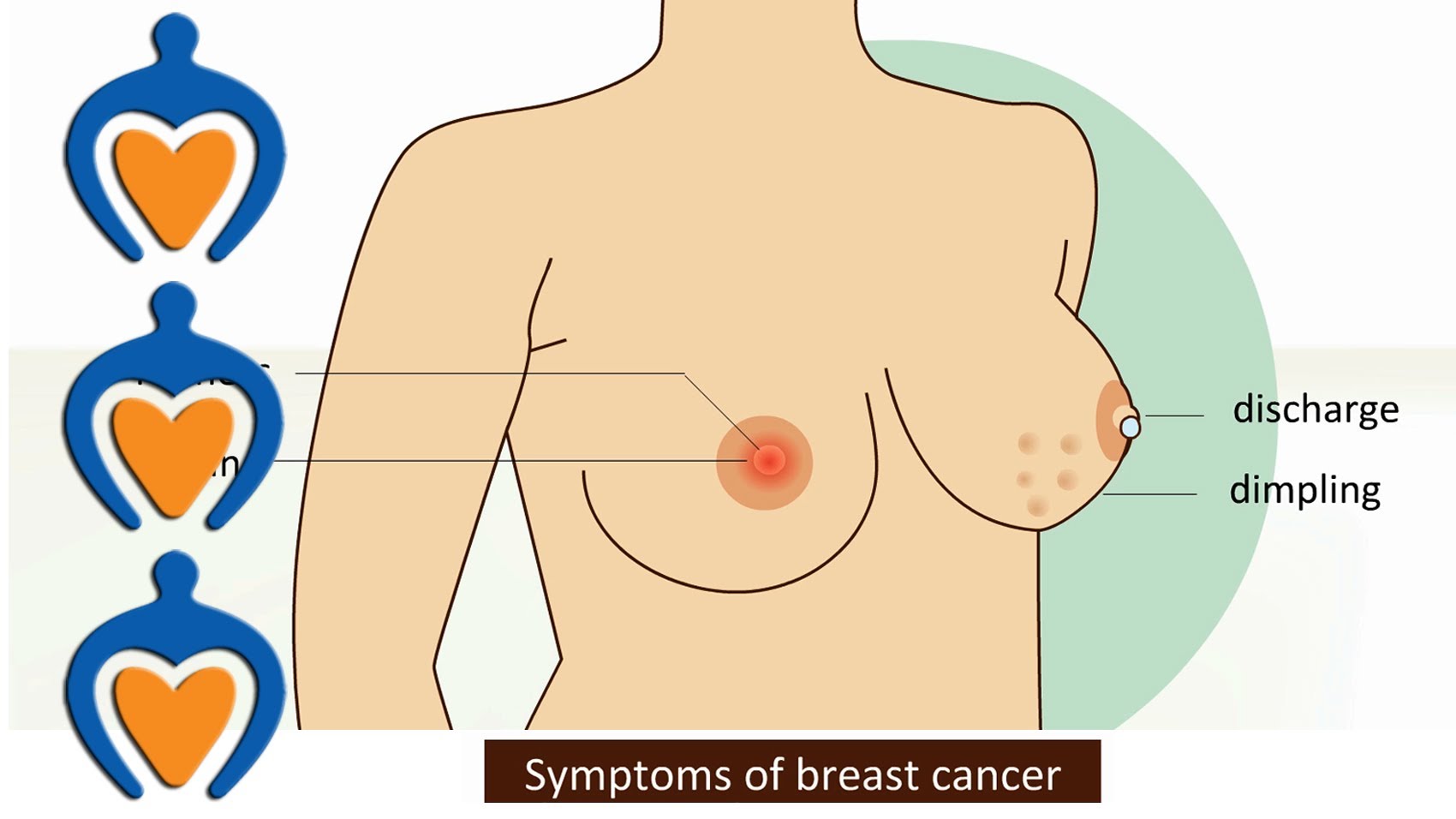
You should see your surgeon if you notice any changes to your breasts such as:
- a lump or area of thickened tissue in either breast
- discharge from either of your nipples (which may be streaked with blood)
- a lump or swelling in either of your armpits
- a change in the size or shape of one or both of your breasts
- dimpling on the skin of your breasts
- a rash on or around your nipple
- a change in your nipple’s appearance, for example, if it becomes sunken into your breast
- pain in either of your breasts or armpits that is not related to your period
The general approach to evaluation of breast cancer has become formalized as a triple assessment:
- clinical examination
- imaging (usually mammography and/or ultrasonography)
- needle biopsy
Your doctor will carry out a physical examination of both of your breasts, including the lump, if any, and may refer you for further tests. Some of the tests that you may have are explained below.
Screening
Regular breast screening is very important because it will help detect any small changes before you have other signs or symptoms. Screening is a way of identifying people who may have an increased risk of developing a certain condition. For breast cancer, screening is carried out using mammograms. This is a procedure that uses X-rays to produce an image of the inside of your breasts.
Mammogram
A mammogram is a simple procedure that uses X-rays to create an image of the inside of your breasts. It is used to help identify early changes in your breast tissue. Younger women usually have denser breasts than older women, which makes changes more difficult to identify. Therefore, mammograms are not as effective in women who are under 35 years of age. If you are under 35, your GP may suggest that you have a breast ultrasound instead (see below).
If you need to have a mammogram, a radiographer (an X-ray specialist) will position one of your breasts on a flat X-ray plate. A second X-ray plate will press down on your breast from above, so that it is temporarily flattened between the two plates. An X-ray will then be taken, which will produce a clear image of the inside of your breast. After the first X-ray has been taken, the same procedure will be carried out on your other breast. A mammogram only takes a few minutes to carry out. You may find it a bit uncomfortable or even slightly painful. After the procedure is complete, the mammogram (the image of your breast) will be examined for anything unusual.
Guidelines for mammogram screenings
- All women above the 35 should have a baseline mammogram.
- All women above the age of 40 are advised to have an annual mammogram until the age of 65.
- You have to know whether you fall in the high risk category. 4. If you have a family history of breast cancer you are likely to be a candidate for genetic testing as well.
Ultrasound
If you are under 35 years of age, a breast ultrasound may be recommended because your breast tissue may be too dense for a mammogram. Your doctor may also suggest that you have a breast ultrasound if they need to know whether a lump in your breast is solid or contains liquid. Ultrasound uses high-frequency sound waves to produce an image of the inside of your breasts. An ultrasound probe or sensor will be placed over your breasts to create an image on a television screen. The image will highlight any lumps or abnormalities that may be present in your breasts.
Needle Biopsy
You may need to have a breast biopsy if the cause of your breast lump cannot be diagnosed using a mammogram or ultrasound. A biopsy is a procedure that involves removing a tissue sample from the lump for further testing. During a biopsy, a fine needle will be inserted into the lump in your breast so that a sample of tissue can be removed. The sample will then be examined under a microscope to confirm the diagnosis.
Stereotactic Biopsy:
If there is any abnormality seen on the screening mammogram films, which the surgeon is not able to palpate clinically, then you are advised to have the biopsy of the suspected area done under mammographic guidance. It is computer aided exercise. The patient actually lies on the mammogram table, and the area of suspicion in the breast is 3 dimensionally targeted (like a missile on the radar operation) and then a small needle is inserted under local anaesthesia. A small amount of liquid is aspirated which is sent for cytology.
Genetic Testing
Approximately 10 to 15 percent of all breast cancers are thought to be familial and about one third of these cases are due to an inherited mutation in a BRCA1 or BRCA2 breast cancer susceptibility gene. BRCA1 and 2 mutations are associated with early-onset breast cancer, and some experts call for aggressive Screening of affected persons.
We are able to offer you screening for your susceptibility of inheriting this genetic disorder through a simple blood test at one our affiliated laboratories.
Who should have a genetic testing done?
- 2 first-degree relatives (mother, sisters, daughters) with breast cancer, one of whom was diagnosed when they were younger than 50
- 3 or more first or second-degree relatives (includes grandmothers, aunts) diagnosed with breast cancer
- Both breast and ovarian cancer among first and second-degree relatives
- A first-degree relative diagnosed with cancer in both breasts
- 2 or more first or second-degree relatives diagnosed with ovarian cancer
- A male relative with breast cancer
Pros and cons of genetic testing
Approximately 10 to 15 percent of all breast cancers are thought to be familial and about one third of these cases are due to an inherited mutation in a BRCA1 or BRCA2 breast cancer susceptibility gene. BRCA1 and 2 mutations are associated with early-onset breast cancer, and some experts call for aggressive Screening of affected persons.
Magnetic Resonance Imaging
In an effort to overcome the limitations of mammography and ultrasonography, MRI has been explored as a modality for detecting breast cancer in women at high risk and in younger women. A combination of T1, T2, and 3-D contrast-enhanced MRI techniques has been found to be highly sensitive (approximating 99% when combined with mammogram and CBE (Clinical Breast Examination) to malignant changes in the breast
Indications for MRI
The high cost and limited availability of MRI, as well as the difficulties inherent in performing and interpreting the studies, require careful recommendations for its use. The following are common agreed-upon and useful indications for MRI:
- Characterization of an indeterminate lesion after a full assessment with physical examination, mammography, and ultrasonography
- Detection of occult breast carcinoma in a patient with carcinoma in an axillary lymph node
- Evaluation of suspected multifocal or bilateral tumour
- Evaluation of invasive lobular carcinoma, which has a high incidence of multifocality
- Evaluation of suspected, extensive, high-grade intraductal carcinoma
- Detection of occult primary breast carcinoma in the presence of metastatic adenocarcinoma of unknown origin
- Monitoring of the response to neoadjuvant chemotherapy
- Detection of recurrent breast cancer
In non-fatty breasts, ultrasonography and MRI are more sensitive than mammography for invasive cancer but may overestimate tumour extent.
Outcome of Screening
EARLY DETECTION OF BREAST CANCER IS THE ONLY PREVENTIVE MEASURE
All the measures of screening, i.e breast self examination, examination by a clinician and Mammogram are aimed at detecting and diagnosing a problem in its nascent phase. The treatment is simple and the prognosis is excellent.