Laparoscopic Anti-Reflux (GERD) Surgery
GERD | Causes | Treatment | Advantages | Before Surgery | Day of Surgery | Procedure
What is Gastroesophageal Reflux Disease (GERD)?
Although “heartburn” is often used to describe a variety of digestive problems, in medical terms, it is actually a symptom of gastroesophageal reflux disease. In this condition, stomach acids reflux or “back up” from the stomach into the esophagus. Heartburn is described as a harsh, burning sensation in the area in between your ribs or just below your neck. The feeling may radiate through the chest and into the throat and neck. Many adults in the experience this uncomfortable burning sensation at least once a month. Other symptoms may also include vomiting, difficulty swallowing and chronic coughing or wheezing.
What causes GERD?
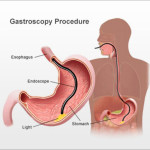
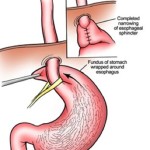
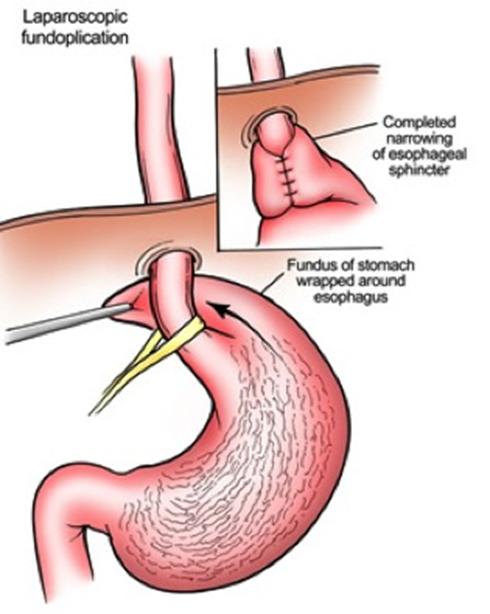
When you eat, food travels from your mouth to your stomach through a tube called the esophagus. At the lower end of the esophagus is a small ring of muscle called the lower esophageal sphincter (LES).
The LES acts like a one-way valve, allowing food to pass through into the stomach. Normally, the LES closes immediately after swallowing to prevent back-up of stomach juices, which have a high acid content, into the esophagus. GERD occurs when the LES does not function properly allowing acid to flow back and burn the lower esophagus. This irritates and inflames the esophagus, causing heartburn and eventually may damage the esophagus.
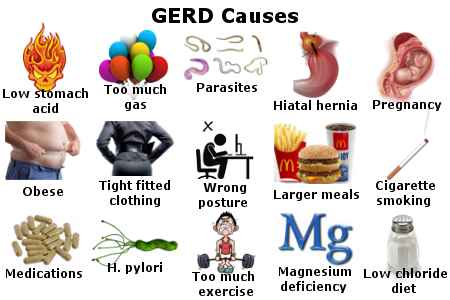
What contributes to GERD?
Some people are born with a naturally weak sphincter (LES). For others however, fatty and spicy foods, certain types of medication, tight clothing, smoking, drinking alcohol, vigorous exercise or changes in body position (bending over or lying down) may cause the LES to relax, causing reflux. A hiatal hernia (a common term for GERD) may be present in many patients who suffer from GERD, but may not cause symptoms of heartburn.
How is GERD treated?
GERD is generally treated in three progressive steps:
- Life style changes:
In many cases, changing diet and taking over-the-counter antacids can reduce how often and how harsh your symptoms are. Losing weight, reducing or eliminating smoking and alcohol consumption, and altering eating and sleeping patterns can also help. - Drug Therapy:
If symptoms persist after these life style changes, drug therapy may be required. Antacids neutralize stomach acids and over-the-counter medications reduce the amount of stomach acid produced. Both may be effective in relieving symptoms. Prescription drugs may be more effective in healing irritation of the esophagus and relieving symptoms. This therapy needs to be discussed with your surgeon. - Surgery:
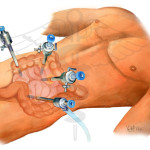
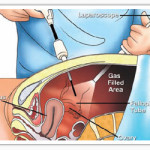
Patients who do not respond well to lifestyle changes or medications or those who continually require medications to control their symptoms, will have to live with their condition or may undergo a surgical procedure. Surgery is very effective in treating GERD.There are procedures being tried, known as Intraluminal Endoscopic Procedures, which are alternatives to laparoscopic and open surgery. You will need to discuss with your surgeon and physician whether you are a candidate for any of these procedures.
Are you a candidate for the Laparoscopic method?
Although laparoscopic anti-reflux surgery has many benefits, it may not be appropriate for some patients. Obtain a thorough medical evaluation by a surgeon qualified in laparoscopic anti-reflux surgery in consultation with your primary care physician or Gastroenterologist to find out if the technique is appropriate for you.
What to expect before Laparoscopic Anti-Reflux Surgery:
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an electrocardiogram, depending on your age and medical condition.
- Your surgeon may request that you completely empty your colon and cleanse your intestines prior to surgery. You may be requested to drink clear liquids, only, for one or several days prior to surgery.
- It is recommended that you shower the night before or morning of the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Stop smoking and arrange for any help you may need at home.
What to expect the day of Surgery:
- You usually arrive at the hospital the morning of the operation.
- Often pre-operative medications are necessary.
- You will be under general anesthesia – asleep during the operation which may last several hours.
- Following the operation, you will be sent to the recovery room until you are fully awake.
- Most patients stay in the hospital the night of surgery and may require additional days in the hospital.
When to call your Doctor
It is important to call your doctor if you develop any of the following symptoms:
- Persistent fever over 101 degrees (39 C)
- Bleeding
- Increasing abdominal swelling
- Pain that is not relieved by medication
- Nausea and/or vomiting
- Persistent cough or shortness of breath
- Pus from wound site
- Any redness surrounding your wound as this could be a sign of infection
- You are unable to tolerate fluids and diet.